Abstract
Introduction The therapeutic paradigm for newly diagnosed multiple myeloma (NDMM) patients undergoing autologous stem cell transplant (ASCT) is evolving. Emergence of newer maintenance therapies has prompted this network meta-analysis to assess the comparative effectiveness of available options using the most up-to-date evidence, and thereby informing optimal therapy in this setting.
Methods MEDLINE and EMBASE were comprehensively searched using a systematically structured search strategy to identify phase II/III randomized controlled trials (RCTs) assessing contemporary maintenance therapies in NDMM patients undergoing ASCT. The main outcomes of interest included progression-free survival (PFS) and overall survival (OS). Precomputed hazard ratios (HR) with 95% CI were pooled using an inverse variance approach. Incidence rate ratios were computed for trials not reporting HR. Mixed treatment comparisons were made using a network meta-analytic approach within the frequentist framework. Relative treatment rankings were evaluated using P-scores (PS) and were interpreted in congruency with pairwise estimates. Higher ranks indicated better efficacy.
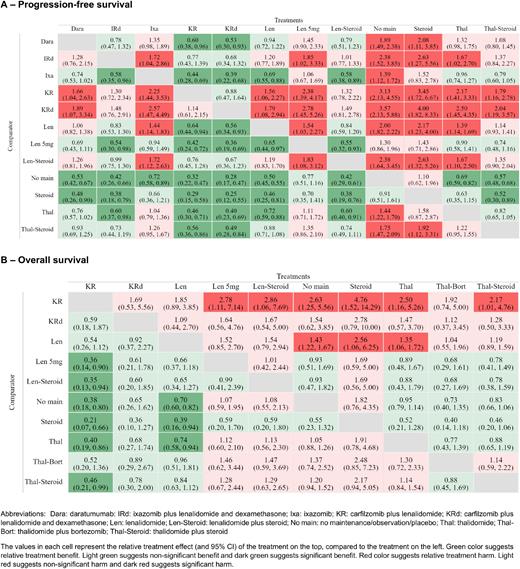
Results As of 25th July 2022, 16 RCTs with 12 unique treatment arms, and 14 RCTs with 10 unique treatment arms, contributed to the network of PFS and OS outcomes, respectively. Mixed treatment comparisons showed that the combination of carfilzomib, lenalidomide, and dexamethasone (KRd) and KR were associated with significantly improved PFS when compared to lenalidomide (Len) maintenance (KRd vs. Len - HR: 0.56; 95% CI: 0.34-0.93, KR vs. Len - HR: 0.64; 0.44-0.94), daratumumab (Dara) (KRd vs. Dara - HR: 0.53; 0.30-0.93, KR vs. Dara - HR: 0.60; 0.38-0.96), thalidomide-steroid (Thal-Steroid) (KRd vs. Thal-Steroid: HR - 0.49; 0.28-0.84, KR vs. Thal-Steroid - HR: 0.56; 0.36-0.86), Thal (KRd vs. Thal - HR: 0.40; 0.23-0.69, KR vs. Thal - HR: 0.46; 0.30-0.71), and ixazomib (Ixa) maintenance (KRd vs. Ixa - HR: 0.39; 0.22-0.68, KR vs. Ixa - HR: 0.44; 0.28-0.69). Although there was a signal of potential PFS benefit with KRd and KR when compared to Ixa, lenalidomide, and dexamethasone (IRd), the difference was not statistically significant (KRd vs. IRd - HR: 0.68; 0.34-1.32, KR vs. IRd - HR: 0.77; 0.43-1.39). The results were consistent for KRd and KR as compared to Len-Steroid (KRd vs. Len-Steroid - HR: 0.67; 0.36-1.23, KR vs. Len-Steroid - HR: 0.76; 0.45-1.28). However, KRd and KR were not significantly different from each other. Ranking analysis showed KRd (PS: 0.95; rank 1) and KR (PS: 0.91; rank 2) were potentially the most efficacious with regards to PFS benefit followed by IRd and Len-Steroid (PS: 0.75, rank 3), Len (PS: 0.63; rank 5), Dara (PS: 0.57; rank 6), Thal-Steroid (PS: 0.49; rank:7), Thal (PS:0.30; rank: 8), and Ixa (PS: 0.28; rank: 9). Len maintenance was associated with significantly improved PFS compared to Ixa (HR: 0.69; 0.55-0.88), and Thal (HR: 0.72; 0.59-0.88) as shown in Figure 1A. Mixed treatment comparisons for OS outcomes showed a consistent pattern of benefit with KR when compared to Thal (HR: 0.40; 0.19-0.86), Thal-Steroid (HR: 0.46; 0.21-0.99), and Len-Steroid (HR: 0.35; 0.13-0.94). Although, there is a signal of OS benefit with KR when compared to Len, the effect is not statistically significant (HR: 0.54; 0.26-1.12). Similarly, while the direction of effect indicated potential OS benefit with KRd as compared to Thal, Thal-Steroid, and Len-Steroid, the difference was not statistically significant. No statistically significant associations were observed for other mixed treatment comparisons with regards to OS at the current follow up of the included trials as shown in Figure 1B. Sensitivity analyses limited to phase III RCTs showed consistent results.
Conclusions Maintenance therapy with KRd and KR may prolong PFS compared to other therapies including Len, Thal, Ixa, and Dara maintenance but not when compared to Len-Steroid and IRd. Overall survival data is still emerging and results at longer-follow up with subgroup analyses by age, prior response status, and cytogenetic risk profiles are warranted and may offer additional insights. Thus, a living systematic review is being maintained and these results will be updated as soon as new data becomes available.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal